RevAssurance™ offers a robust set of resources, including 400+ templates, Denial Topic Encyclopedia pages, and Rebuttal Scripts all designed to help your team resolve denials quickly and accurately. With access to every Jurisdiction and state-level customized tools, your staff will be able to respond confidently to the most complex of payor disputes. Our platform supports your efforts in accelerating cash flow, reducing bad debt write-offs, and patient satisfaction by streamlining denial management and optimizing recovery.
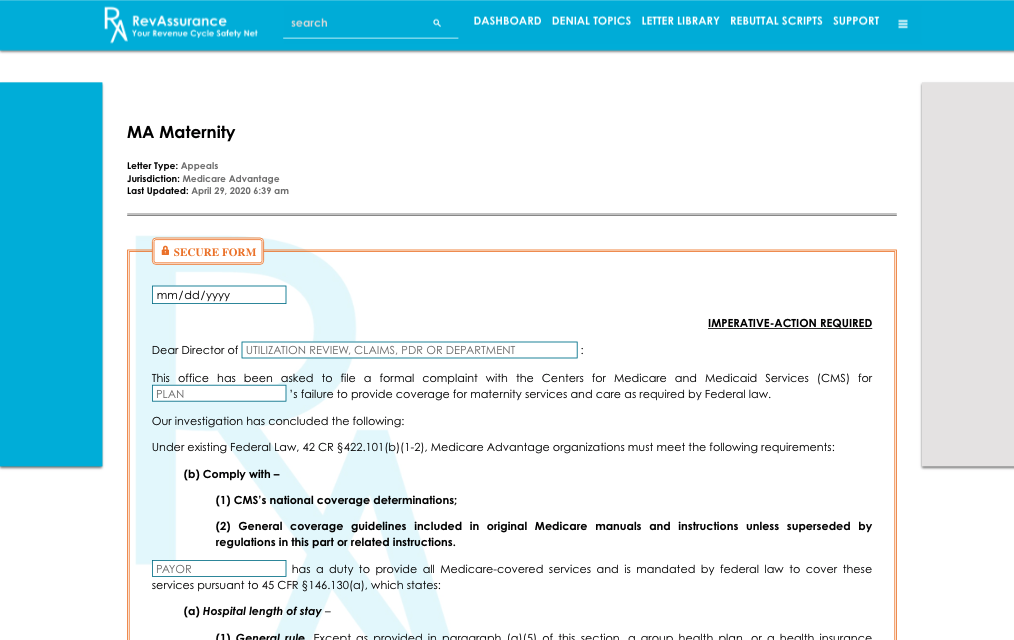
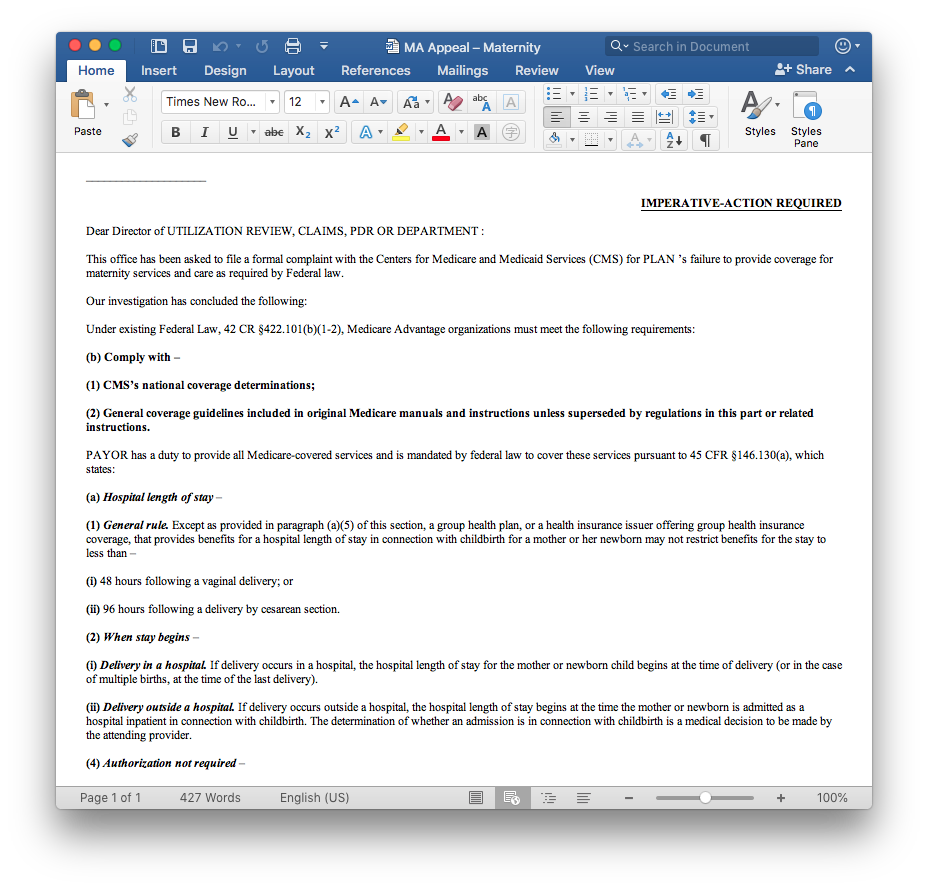
Simply input the claim details, and the platform will automatically generate a professional, tailored appeal letter in Microsoft® Word format.
RevAssurance™ provides tailored appeal templates for every payer jurisdiction, ensuring your team can effectively address payer disputes across both state-specific and federal regulation.
Our Jurisdiction Map streamlines the process by offering real-time access to up-to-date contact information for state and federal regulatory agencies, enabling your team to easily file complaints or escalate disputes as needed.
Each page of the Denial Topic Encyclopedia provides targeted resources to help your team navigate payer disputes. We cover key denial scenarios and improper payment tactics, offering tailored solutions based on payer type and jurisdiction.
Automatically generate appeal letters when payer responses are unhelpful
Pre-written responses for phone calls and meetings with payors
Follow up with a formal affidavit to strengthen your position
Access relevant statutory, regulatory, or case law to support your case
Easy access to file complaints with the appropriate agency
When you’re faced with payer disputes, swift and clear communication is essential. Rebuttal Scripts equip your team with the right tools to address payer defenses effectively, ensuring that you respond with confidence and accuracy.
Hold payors accountable for their responsibility to comply with prompt payment laws, while clearly outlining the next steps in the compliance process for timely resolution, empowering your team to take charge of the situation.

"ERN continues to deliver on our commitment to simplify healthcare payments, giving providers the confidence to focus on what matters most: their patients and communities."
